Access to medical oxygen remains one of the most critical needs in primary healthcare. For newborns in distress, mothers facing complications, and patients struggling to breathe, oxygen is not just a treatment; it is a lifeline. Yet in many counties across Kenya, dependable access to oxygen has long been inconsistent, unpredictable, and often prohibitively expensive for families who need it most.
In numbers.
Globally, pneumonia remains the leading infectious killer of children under five, causing more deaths, yet oxygen therapy can reduce pneumonia mortality by up to 35% (UNICEF & WHO). According to a 2015 report on neonatal deaths in Kenya, newborns are particularly vulnerable, with birth asphyxia and complications of prematurity contributing to nearly half of neonatal deaths in Kenya, conditions in which oxygen is required immediately and consistently.
Despite this need, fewer than 50% of health facilities in many African countries have reliable access to oxygen, and up to 70% of donated oxygen equipment becomes nonfunctional within 3 years due to limited maintenance and technical capacity (PATH, 2021; WHO Medical Device Report, 2018). Evidence shows that pairing oxygen equipment with ongoing health worker training dramatically improves survival outcomes, reducing hypoxia-related deaths and minimizing misuse or wastage (Lancet Global Health, 2020).

Health system strengthening
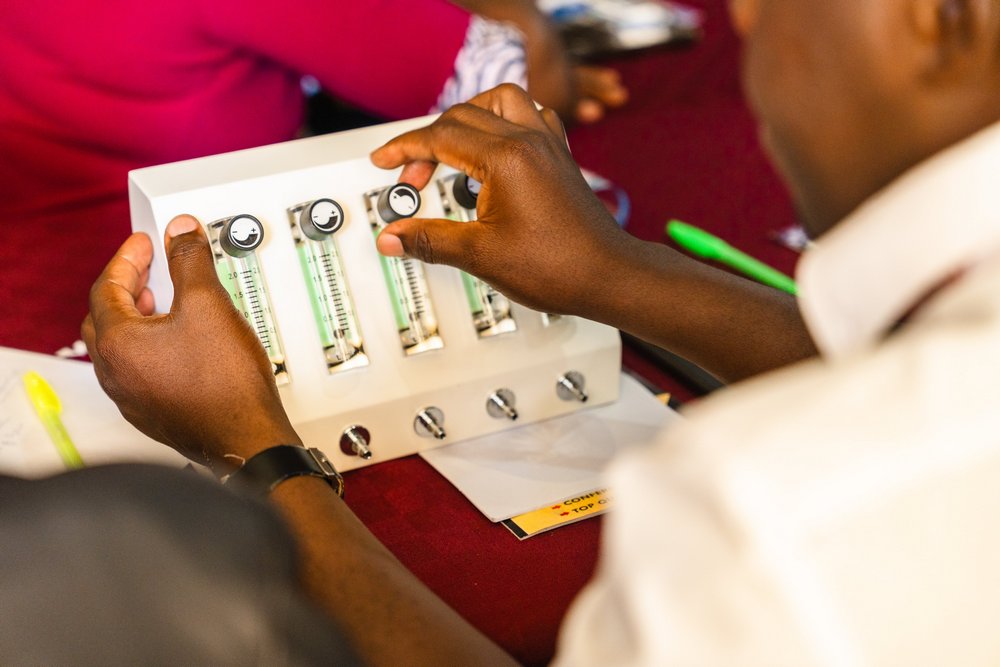
These realities have shaped our Oxygen-as-a-Service (OaaS) model, implemented with Better Future COLAB. Our work in Homabay and Busia counties has been particularly illuminating, providing key lessons on building resilient oxygen systems that serve communities effectively.
In these counties, challenges were apparent; health facilities frequently experienced prolonged oxygen shortages due to irregular deliveries, limited maintenance capacity, and equipment that remained unused or malfunctioned.
“Health workers often knew to save lives but lacked the tools to do so. Families sometimes had to travel long distances or pay high costs to secure oxygen for critically ill loved ones. These realities underscored the urgent need for a holistic model, one that goes beyond equipment donations to strengthen the entire ecosystem of oxygen delivery,” said Michael Njuguna, OaaS Project Lead.
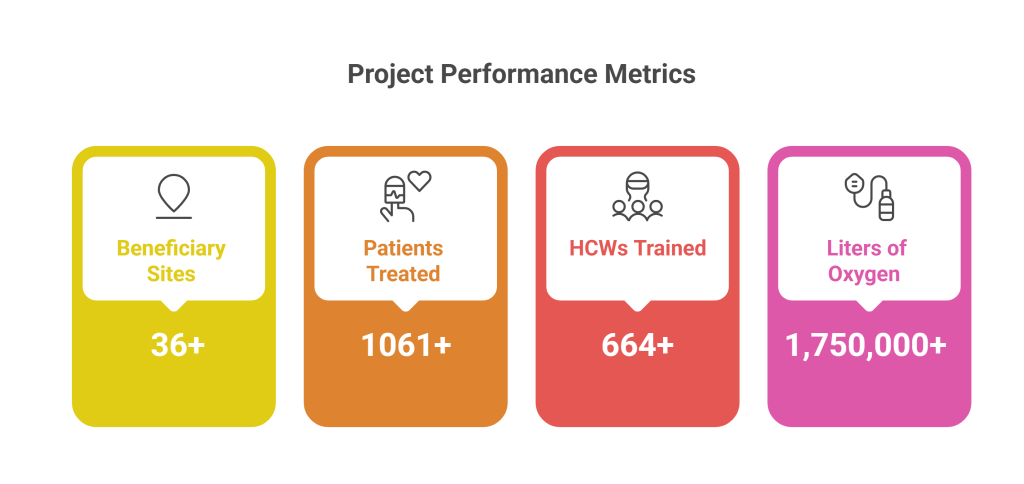
Our Metrics
Through his technical support, the OaaS model has demonstrated the impact of combining reliable supply, training, and technical support.
“We have seen over 36 health facilities in Homabay and Busia now consistently receive functioning oxygen equipment, and about 1,061 patients have benefited from timely access to oxygen therapy,
Additionally, CPHD has had over 664 health care workers trained to administer oxygen safely and manage respiratory emergencies and over 1,750,000 liters of oxygen delivered, ensuring critically ill patients receive the care they need when they need it.
Successively, health workers now respond faster to emergencies, avoid unnecessary referrals, and gain community trust as oxygen becomes a reliable resource rather than a scarce commodity.
Progress in Homabay and Busia proves that when systems, people, and partnerships come together, reliable oxygen access becomes achievable and sustainable. As CPHD and Better Future COLAB continue scaling this model, the lessons learned will guide counties across Kenya in building stronger, more resilient health systems.